What is naloxone? Learn about the overdose reversal drug
This page will tell you everything you need to know about naloxone, how it could help you to save someone’s life, and how to get a free kit.
What is naloxone?
Naloxone is a drug that can reverse the effects of opioids, such as heroin, methadone, opium, codeine, morphine, and buprenorphine. A naloxone dose can even save someone’s life if it's used quickly after they’ve overdosed on opioids and before emergency help arrives.
The effects of naloxone don’t last very long, so it’s important to always call 999 and ask for emergency help when you use it.
Synthetic opioids are a new type of drug that are very strong and very dangerous. They have been found in other drugs across the UK, so people might not know they are taking them.
If you think someone is overdosing but you aren’t sure what they’ve taken, you can still give them naloxone. It won’t hurt them and it could help them.
Get a free naloxone kit and training
If you'd like a naloxone kit, visit or get in touch with your local service. A trained member of staff will give you a kit, and teach you how to prevent and manage opioid overdoses. Naloxone training can take as little as 10 minutes.
Medical professionals have been using naloxone in emergencies for many years. We want to make sure that anyone who needs it has it to hand and knows how to use it.
Anyone can use naloxone in an emergency. You don’t need to be a doctor or medical professional. We give kits to anyone who could use it to save a life, for example, if you use opiate drugs or if someone you know does.
If you use our services, you can ask for a few extra kits to give to people you know personally. You must be trained to an enhanced level so you can pass on the training to the people you give the naloxone kits to.
Carrying naloxone and knowing how to use it could help you to save a life.
If you use your kit, or if it is lost, damaged or out of date, we’ll be happy to give you a new one.
How to use naloxone to save someone’s life
If someone has had an opioid overdose, naloxone will only reverse the effects for a while. After 20-40 minutes, the effects will wear off and the person will go back into overdose.
Always dial 999 and ask for an ambulance straight away after giving someone naloxone.
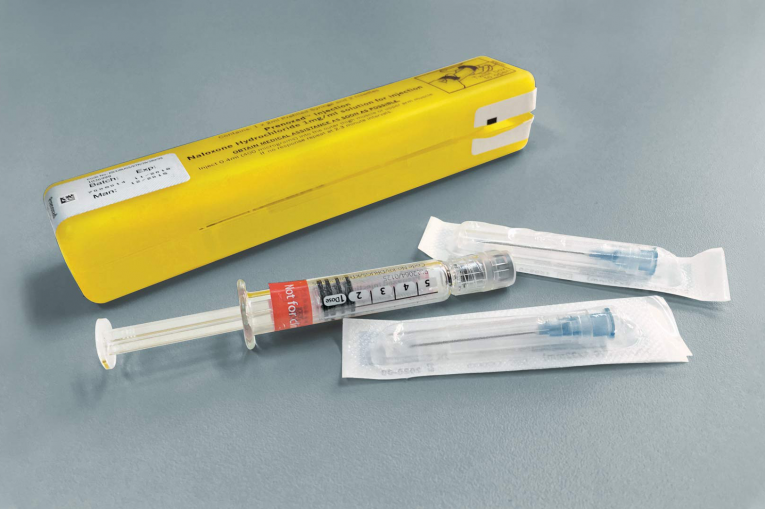
Naloxone kits come in two types. They have the same effects but you use them differently:
Prenoxad, which comes as a pre-filled syringe. You inject this type of naloxone into a person’s leg, through their clothes if you need to.
Nyxoid, which comes as a nasal spray. You spray this type of naloxone into a person’s nostril.
What to do if someone is having an overdose
Keep calm and follow these steps:
- Make sure that you’re not in any danger first. Keeping yourself safe is important.
- Call 999 and ask for an ambulance.
- Check to see if there is anything obstructing their airways.
- Place the person in the recovery position. You can find out how to do this here.
- If you have Prenoxad, inject it into their thigh or upper arm muscle.
- If you have Nyxoid, place the spray in their nose and press the plunger.
- Wait with the person until the ambulance arrives, and give the used naloxone kit to the paramedics.
When you use naloxone, you should see it start to work in two to three minutes. If the person has not responded after that time, give them another dose and wait for two to three minutes again. The effects of naloxone will last for 20-40 minutes, but after that, they will wear off and the person will begin overdosing again. It’s important that the person gets medical help during this time.
Naloxone is only effective for opioid overdoses, and won’t work with any non-opioid drugs. You should never use it as a safety net to take extra risks.
If I didn’t do it, I knew he would die so I gave him two doses.
How to tell if someone has overdosed
Keep an eye out for these signs that someone is having an overdose:
- Deep snoring/gurgling noises
- You can’t wake the person up, and they don’t respond if you shake their shoulders or call their name
- A blue tinge to the lips, nail beds or other extremities
- They have stopped breathing.
Find out more about recognising an overdose
You should always call 999 if you think someone is having an overdose.
Don’t be scared that you’ll get in trouble. The ambulance will not bring the police with them except in very particular cases.
You can find out more about naloxone at Naloxone – Naloxone Saves Lives.